The Scheduling Conundrum
Direct scheduling remains an enigma, wrapped in a mystery, surrounded by a conundrum. Why?
This post is a joint production brought to you by the Health API Guy (Brendan) and Health Tech Stack (Jan-Felix) - you should definitely be subscribed to both! Tremendous thanks to Julie Yoo, Joe Mercardo, Erica Jain, Krish Maypole, Morgan Blumberg, Samir Unni, Shashin Chokshi, and Colin Keeler for their invaluable input.
For almost all of humanity, our primary healthcare goal is to never be a patient. We seek to live our normal lives working and playing and doing whatever pursuits might fulfill us in our time on this planet. However, the wears and tears of our activities, the bad luck of chance, and other factors inevitably mean that we do become patients - we seek a checkup, we need urgent care, we identify a need for a medication, a procedure or a diagnostic.
At that precise moment (paraphrasing the words of Eric Andre) we all just want to be let in. We want to be able to see the exact person who can fix our problems or at least make us as close to whole again as possible. We want that to happen as quickly, easily, and cheaply as possible.
But...this is easier said than done. Appointment scheduling is the epitome of the dysfunction of the American healthcare experience, the purest distillation of an unending onslaught of frictions, missed handoffs, and varying failures. In particular direct scheduling, i.e. the ability for everyone to see when a doctor is available and book an appointment, is rarely adopted.
Fixing this is a big, hairy, audacious goal, so it’s no wonder that many have tried and many will try. The past month alone (detailed here in Brendan’s thread) has seen an incredible amount of change on the scheduling front. Brendan and I got together to talk a bit about the why (root causes and incentives), the who (existing players), and the how (where we think things will go and businesses will be built).
Why should schedules be open?
Direct scheduling is common practice in almost every industry: you can book airline tickets online, you can make restaurant reservations, and you can schedule workout classes. Calendly even brought this to practice to person-to-person schedules.
It’s not rocket science to imagine that patients want the same ease of access and consumer experience brought to bear for doctors’ appointments. There’s an inherent urgency to health problems - finding the intersection of speedy resolution and quality care is what we all want as patients. Extrapolating this further, there are myriad reasons (and even built-in incentives) for us to expect this to already exist in healthcare:
For Patients
The value proposition for patients is clear: convenience! We all have busy lives - we want to fit the doctor’s appointment into our schedule. Also, Gen Z (and maybe even millennials) simply avoid making calls on their phone like the plague, strongly biasing towards apps, websites, and text engagements. There’s no better way to forcibly eject younger generations from your onboarding and acquisition process than by putting them on hold. Without digital interactions that they can access 24/7, businesses are distinctly disadvantaging themselves against their competition.
For Physicians
Pure play forces of our grand capitalistic economy would suggest that doctors would want direct scheduling. Simply put (or oversimplifying tremendously), a practice can earn more revenue by treating more patients - and treating more patients requires more optimized utilization. This is true for both the fee-for-service world (more patients = more procedures = more cash) and in a value-based care world (better utilization = bigger patient roster = more capitation payments). Opening up their availability to a broader audience would presumably help doctors fill open slots that might otherwise go unused.
In addition, direct scheduling hypothetically reduces admin burden on the staff needed for making and taking phone calls and shifting appointments around.
As an aside - Short waitlists and easy scheduling are literally some of the core benefits most people list if you ask them why single-payer or other alternative healthcare strategies won’t work in America, so it’s actually quite ironic how shitty the current situation is with that in mind.
From a more altruistic perspective (those do exist in healthcare!), optimally utilized physicians could actively provide more and potentially better care. Automatic routing of care would enable physicians to focus on “specialized, high-acuity care” and appropriately route lower-acuity care to navigators, coaches, or providers more appropriately credentialed, theoretically without human interaction required to book.
For Referring Physicians
Direct scheduling would also make it much easier for primary care physicians to get their patients to see specialists for preventative visits. If the primary care doctor can schedule a follow-up appointment directly at the visit, the care continuity is maintained for the patients. The friction of scheduling is work for the patient that few enjoy or relish. Currently, scheduling a follow-up appointment is a barrier (the numbers don’t lie). The higher the barrier for the patient, the less likely they will be to actually show up at necessary screening appointments. The more engaged primary care providers are currently handling this for their patients, but only with more manual overhead and boots on the ground: calling specialists to see whether they have availability, handing off the patients to care navigators, or staffing a team of referral administrators. The less engaged, however, just hand out a bunch of business cards (with QR codes, even, if they’re fancy). Whether the specialist takes new patients and is available in a reasonable time frame, is up to the patient to find out.
For Payers (selectively) & Care Navigators:
More and more payers try to actively steer their patients to cost-effective providers. They have invested deeply in analytics solutions to identify those preferred providers in their network and now they are trying to steer their patients towards those providers. Direct scheduling is a logical way to make it easier for their members to access their preferred providers through the payer portal (a thesis that seems to be shared by Kyruus in their acquisition of HealthSparq). Employer-facing care coordinators such as Accolade, Rightway, Transcarent, or Collective Health also offer these concierge services for finding and scheduling appropriate care, and direct scheduling would reduce their manual tasks. Today, care navigation is heavy analog work requiring phone calls and faxes ad nauseum, solved simply by increasing staffing. Direct scheduling largely turns this ongoing services investment into more automation and allows care navigators to focus simply on finding the best possible providers.
Well - so why is direct scheduling not an industry standard?
“Wow, Jan-Felix and Brendan” you might say, “so many good points here. You’re so smart and talented. It feels objectively and abundantly clear that direct scheduling is in everyone’s best interest. So why isn’t that the case?”
Great question, valiant reader. The fact of the matter is that despite the weight of the incentives above, there are equal or greater headwinds historically to ubiquitous accessibility on a national scale.
Problem 1: Triage - “Risk of seeing the wrong patient”
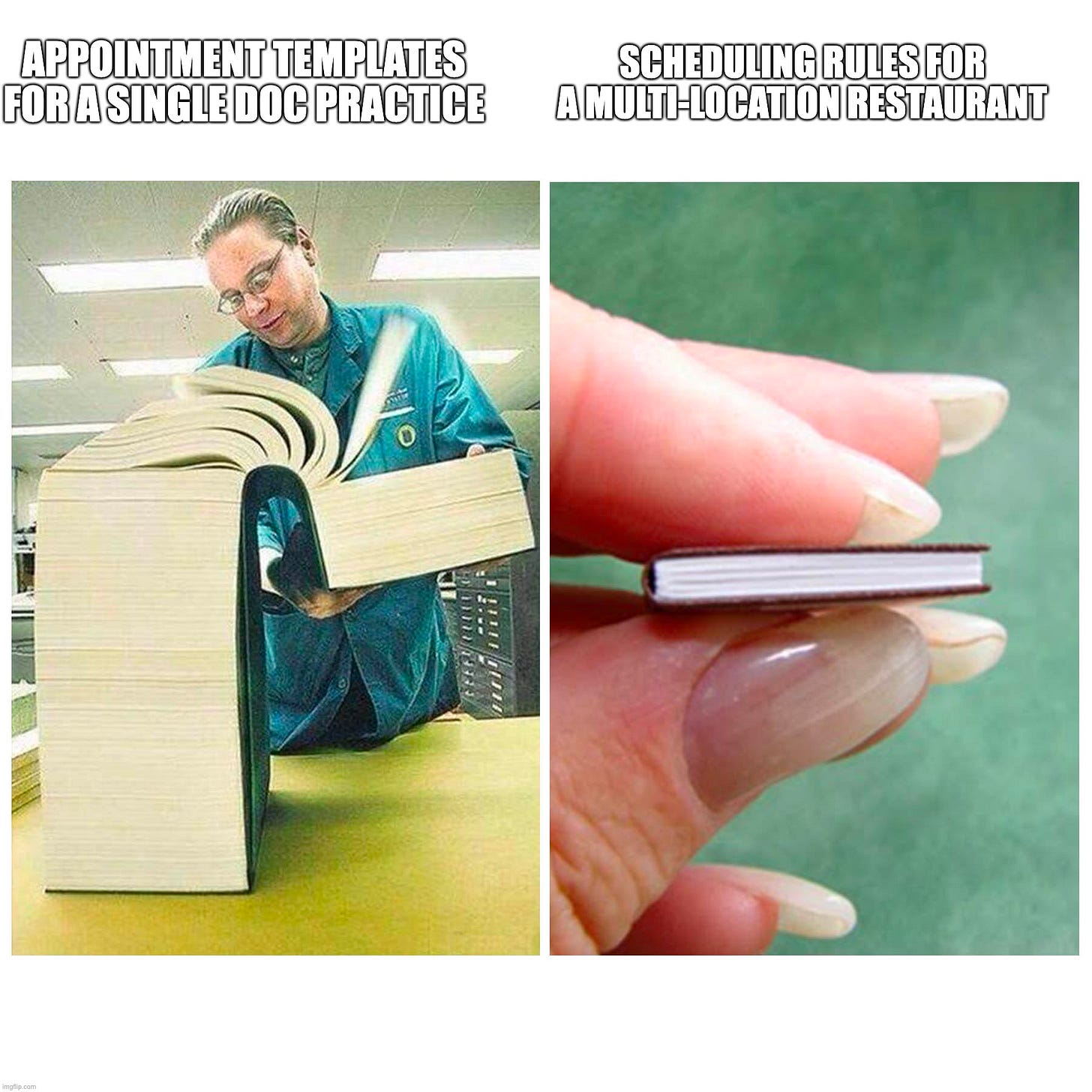
While some restaurants may limit their clientele based on dress code or other factors, generally speaking, any given customer is equivalent as long as they have a willingness to pay. In this regard, scheduling a doctor's appointment is very different from making a restaurant reservation - not all customers are equally appropriate.
First of all, a missed appointment is much more costly in healthcare than for a restaurant, as there are usually not enough walk-ins to fill the space. Therefore, there’s a strong prerogative for providers to be 100% sure that when they have scheduled a patient, they actually will see that patient. There are more than a few factors that need to be cleared before the visit:
Insurance Coverage: Is the provider part of the insurance network of the patient?
Prior Authorization: Is a prior authorization needed and has it been approved yet?
Referral: Is a referral needed and has it been received yet?
Specialty Match: What is the reason the patient is coming in? Is the doctor the right person to see the patient? This is especially important for sub-specialties. For example, an electrophysiologist is technically a cardiologist, but will not see patients for medication management. These subspecialists are especially protective of their calendars.
Experience Match: The body of work (and volume of work) of the physician correlates to the outcomes of that care. How does a patient get matched to the provider with the right experience for their acuity? The example Julie outlined years ago still resonates here.
SDOH and Intangibles: Do they speak the same language as the patient? Is the patient able to get to the provider?
Most of these checks are done manually and laboriously today. Scheduling process optimization via technology isn’t necessarily a core competency of providers - they are comfortable doing them this way. Change inherently has some risk of missed income and wasted time.
Problem 2: Visit Type Matching
A restaurant typically doesn’t have a variety of different types of experiences to choose from. A restaurant booking may have sub-divisions for table size, indoors/outdoors, or some small features. Likewise, although hotels may have different room types, there isn’t a ton of nuance beyond that - a better room is roughly correlated with increased price, without other dependencies or sub-classifications.
The opposite is true in healthcare. Each visit is a complex web of matching patients with the visit type appropriate to the exact moment in the patient’s journey. Even if the patient is correctly matched with a provider, they will now need to be matched with a certain appointment type.

The easiest appointment type is an initial consult, as it is quite standardized and many providers actually allow direct scheduling for this visit type. However, it only gets harder from here. For other visits, like procedures and treatments, the doctor will need to allocate different amounts of time, and will need to make sure facilities & equipment are available and they might need to order drugs and tests before the visit. Imaging centers provide a great example - even though ordering an image may seem simple, there are quite a few specifications on what type of image type needs to be performed and sub-divisions of those image types, such as with or without contrast.
What makes this even harder: every organization has its own flavor of appointment types. This means that it is quite hard for an outsider (even for a medical professional) to discern what the right visit type is actually correct to book. For this reason, most practices gate their appointments via the front desk, a shadowy priest class present at every healthcare institution who have memorized and studied the tribal knowledge and who alone can divine an appropriate time to see the professionals they represent.
Problem 3: Fluid calendar - patients and operations are unpredictable
It’s like clockwork. A practice starts the week with a perfectly planned calendar, a beautiful work of art balancing patient types and conditions, with the right breaks for charting and lunch. But by Monday afternoon, everything has changed - the schedule is a minefield geared into hyperdrive, long days laden with overlapping appointments, interruptions, and no breathing space. Doctors’ calendars need to allow for quite a bit of flexibility for several reasons:
No-shows & Rebookings: You’d think the urgency and acuity of healthcare might mean people fulfill their promises and show up when they say they will. You’d also be wrong. Patient’s fear of needles, logistics of getting to the provider’s location, and other factors all combine into relatively frequent no-shows and rebookings. This is especially prevalent when coming from online scheduling services (like ZocDoc) and/or when no prior relationship exists. As a result, some practices copied the practice from airlines to double book or overbook their day or allow for walk-ins and waitlists to fill the open slots.
Appointment lengths: Appointment lengths are also not always predictable - certain procedures can take much longer than expected if acuity is not judged properly or an emergent condition is uncovered. Like a butterfly flapping its wings, this has a ripple effect cascading into a hurricane throughout the whole calendar. This can mean that some appointments need to be rebooked, decreasing patients’ trust in the provider.
Acuity: Some doctors keep capacity open for acute patients. While many procedures can be planned well in advance, often patients need care on the same day or week. Handling these types of patients requires quite some appointment juggling.
Problem 4: Control & Doctor Preferences
Besides the hard business factors, there are also soft factors for doctors on what constitutes an optimal schedule. They range from easy preferences like “I don’t want to see patients on Friday afternoon so me and the boys can hit the range” to complex scheduling logic “I would like to schedule patients only consecutively starting backwards from 2 pm” to hyperspecific logic predicated on incredibly nuanced patient attributes, like “I would like to not see two highly emotional patients in a row”. A lot of these preferences live in the schedulers’ brains and are internalized over a long period of time (the aforementioned tribal knowledge above). As a result, it is quite hard (and perhaps impossible) to codify those intangible preferences into machine computable logic.
Problem 5: Why see more patients?
Many doctors have more patients than they are able to handle and they have long waitlists. This is especially true for doctors with strong established relationships in their community or that have a good reputation and/or low coverage of their specialty in their region. These providers are obviously fine with the current way appointments are scheduled and lack an incentive to move to more modern processes. In fact, gatekeepers and scheduling barriers might even be desired to control the flow of new patients!
Even for PE-owned and hospital-owned practices, the incentives for taking on more patients and fully utilizing the time is not a given. Often compensation schemes are salaried and not based on the number of patients a doctor sees, further degrading the incentive to squeeze in more appointments.
Problem 6: Relationship & patient preferences
There are many people in this world with different preferences; thus, a phone call is a communication medium that some populations of patients (and their providers) actually still prefer. The highest cost patients are usually in their 70s and older. This population distinctly lacks the adverse attitudes toward phone calls that millennials and Gen Z have. They are not savvy with text or typing, they don’t download applications as frequently, and they default to conversation to solve problems. For providers serving Medicare or other groups of patients, relying on phone calls is actually the optimal way to maintain the relationship with the patient and keep them engaged.
Beyond that, there are other preferences that complicate scheduling, such as cultural factors. Few of these outreach solutions have multi-language support, which is especially important among physicians serving communities in which English is a second language.
Problem 7: Integration sucks
Last but not least - setting up this particular workflow with EHRs is really quite tough, at least until recently. You need availability synced to you, but few EHRs supported a query model to pull this in real-time historically. Synchronizing appointment templates is one option, but what if Dr. Smith gets sick or plays hooky to go hit golf balls? EHRs also have historically pushed back on multiple sources of truth for scheduling, so while writing appointments back into the EHR has had broader support technically, there have often been hoops to jump through. Redox literally has a whole white paper dedicated to this topic, suggesting it’s problematic enough to warrant marketing their solution.
Market Map - how providers are trying to address this
Disregarding all of these challenges, several fearless vendors are trying to address this problem and open up doctor’s schedules for you!
Here are the different approaches:
Consumer-Facing: The main value proposition of these consumer-facing companies is offering new patient leads for the health care providers. Aside from some aggregators that rely on advertising, they usually charge the provider a fee for each patient that enters the doctor’s office through their platform. One fundamental challenge of these tools is that patient acquisition costs are usually a one-time cost vs. a recurring line item. As described earlier, doctors have to do marketing until they don’t have to do it anymore. Building a strong provider value proposition beyond that is often something these consumer-facing companies are not well-equipped to do.
EHR & Practice Management Systems: More and more EHRs and Practice Management systems added features to their platforms that allow doctors to open up their schedules and generate links that can be embedded into websites or other applications. For the vendors, this is a way to charge the provider for another feature (as always). For the providers, this is often the easiest way to get more patients into the door without having to add another tool to their stack.
Patient Engagement Platforms: Most EHR direct scheduling solutions are quite primitive and don’t address all the challenges described earlier. That’s why many point solutions emerged that try to offer a better scheduling experience for patients while electronifying the gatekeeping functions of a front desk scheduler. These SaaS or license-based tools are very common for practices that care about their patient experience and brand, such as digital-first health companies and concierge-like care providers.
Health System Platforms: While similar to patient engagement platforms, organizing the schedules of a health system in order is another beast. These companies specialize in the overwhelming complexity of large health systems and integrated delivery networks. The value proposition of these platforms is (1) improving the utilization by standardizing appointment types across organizations and (2) reducing patient leakage by making schedules available within the organization.
Opportunities and Outlook - our “Hot Takes”
The recap and restatement of the status quo are all fine and good, but what does this mean for the future? Whether by the will of the government or the relentless but capricious forces of the free market, will we see easier appointments we all desire? What businesses will be built and where will legacy parts of the industry crumble to dust? Don’t worry, fam, we got you.
With the current trajectory, the quest for direct scheduling seems on the precipice of massive second-order regulatory tailwinds. The CMS Prior Authorization API Rule and accompanying ONC regulation seem to be coming at some point (detailed in Brendan’s article). Barring massive changes, none of this actually addresses scheduling head-on, but electronic prior authorization would mean one of the biggest barriers to easy appointments may fall. Additionally, EHR API requirements in Cures do not call out scheduling, but the shift to the FHIR economy has already resulted in some of the top EHRs creating availability APIs, a feature never before available in the HL7 world. We’d like to see the industry converge their approaches here, though, as many EHRs are creating different FHIR-based direct scheduling implementations.
This will enable quite a few new business opportunities which new entrants and existing companies are racing to capture. A first observation is that health system platforms and patient engagement tools will pivot into acting as “First Mile Aggregators”. Health system platforms and patient engagement tools already do the hard, thankless groundwork of getting a practice or health system’s schedule in order and automating their intake, and triage process. We expect most of these players to shift and develop or open up their APIs for other companies to integrate with. This will allow them to not only monetize through a license fee with their providers as they do today but to resell capacity/availability to other businesses (more on that in a second).
This trend is already happening today, as we see NexHealth, whose initial wedge was delivering patient engagement tools to dentists and small practices, but has created an API program and repositioned itself as an integration solution for dental applications like SmileDirectClub and Quip. Kyruus seemingly also is in the midst of this transformation, opening up the schedules of their customers to aggregators such as Google. This is a great way for these companies (where Business Agreements allow) to upsell the work they’ve already done, so we predict that more will be making the move towards becoming a first-mile aggregator and exposing their scheduling capabilities.
We think this shift will be challenging for a lot of vendors. It’s a truly different core competency to create an API and the surrounding developer ecosystem than it is to create SaaS tooling for providers. It’s also an entirely different sales muscle - will the existing sales team with their Rolodex filled with health systems and practices be equipped to actually sell to digital health vendors, payers, or other businesses? Regardless, the health system platforms and engagement tools that can pull this off will skyrocket in their value to the overall ecosystem.
So if more schedules are accessible, who will be picking up this capacity? Let’s first look at the consumer-facing companies. The first, of course, is Google. After so many failed attempts at breaking into health care in areas that were firmly outside their core competencies, have they finally found a wedge into the field? We think this fits the model of success they’ve found in other industries and they have a playbook called the Google Squeeze. In their first stage, given that they are uniquely positioned in their large pre-existing monetization of attention through ads, they will be willing to pay providers & first-mile aggregators to list their schedules on their platform. Once established as the to-go place for finding doctors and the first touchpoint of the patient relationship, their playbook entails that they may look to cut out the first mile aggregators. Eventually, they could start charging doctors for patient leads (or at least be in a position to drive up provider advertising prices). That possible future entails true patient steering power that most healthcare payers can only dream of.
ZocDoc is another candidate to aggregate the first-mile aggregators for consumers, with a huge head start as one of the first digital health companies and a large pre-existing provider footprint. However, their current business model (charging providers pay-per-lead) might not work as well with Google as a competitor that sits at their top-of-funnel on the demand side. The strange and twisted beauty of ZocDoc is that it tries to live in many worlds: building first-mile scheduling integrations, existing as a consumer-facing brand, and now selling to other businesses via API. Can one company actually be everything everywhere all at once to all people?
There are also many interesting B2B use cases for integrating with these first-mile aggregators:
Provider data aggregators already sit closely in the workflow preceding scheduling. It seems logical that they might take that next step and attempt to upsell their existing customer base by buying or developing this capability.
As noted earlier, payers and care navigators are quite interested in surfacing scheduling and availability information through their patient portals. This could improve patient steerage to the providers they deem more cost-effective while reducing their ongoing linear investment of new schedulers down to the less expensive, fixed cost of an electronic solution.
Digital health companies are another logical candidate, as they want to deliver a great consumer/patient experience. To that extent, direct scheduling and availability of information provide a more seamless experience when they have to refer patients out to in-person doctors.
A world built on the foundation of direct scheduling has a variety of exciting derivative business opportunities:
End-to-end referral collaboration: True interoperability is not just about patient data transfer and chucking a CDA over the fence to your neighboring physician. It’s the radical enablement of doctors in different organizations to work together on a patient’s care in novel ways unthinkable in the pre-digital era. However, we have thrown in so many stones in form of the administrative burden of prior authorizations, fax machines, and call centers that this path of collaboration is nigh unimaginable. Thus, we sit in the era of Digital Health 1.0 digitizing legacy patterns and processes, but direct scheduling is a critical piece in the leapfrog moment to our next era: one of effortless provider collaboration. It may take a witch’s stew of provider directory vendors, direct scheduling solutions, patient data interoperability tools, task management platforms, prior-auth & eligibility APIs, payment rails, and patient communication solutions, but we believe this frothy mix will converge into an end-to-end referral tool that will cause us to question the simple software we’ve built in previous eras.
Digital Care Navigators: If direct scheduling will be a thing, care navigators that are selling to employers could be in a tough spot. Their current operating model is pretty much based on call centers that research providers and schedule appointments for their members. Direct scheduling will give rise to fully digital and automated care navigators. Maybe that is what Comcast had in mind when dumping Accolade earlier this month... or maybe there was another reason, but this is one sector of the industry that faces massive, irrefutable disruption as nationwide availability comes into being.
Conclusion
Simply put, this is an exciting time to be alive. Market and regulatory trends point to a rosier future than the decades that have passed and digital health is ascendant. If you’re working in this space or found this article interesting, we’d love to chat with you and hear more - you can reach us on Twitter or by replying to this email (if you’re subscribed). And if you’re a provider, EHR vendor, or government regulator, we all have just one simple ask of you:
Let us in.
If you want to learn more about this topic, try:
Sandy Varatharaja’s take on scheduling challenges
Mark Olschesky’s overview of scheduling as part of the interoperability problems
Julie Yoo’s talk about the fragmentation of health care schedules










Great overview of a complicated and archaic process. Pretty cool to see the efforts happening in this space.
Three points to add
1. An interesting segment of healthcare as it relates to scheduling- urgent cares (UC). Their main innovation was combining the walk in nature of the ER with accepting only low acuity illnesses and injuries as are seen in primary care. Main benefits of walk in include not having no shows and patient convenience. Main limitation is unexpected wait time. From my experience, a lot of patients value the convenience of walking in whenever they feel like it and are willing to deal with unexpected wait time because if they wait too long then they’ll just come back another day or time when the wait is shorter.
2. As for the science of scheduling, another thing I’ve learned about is AI and predictive scheduling. There are programs which calculate how likely a patient is to no show and thereby allow the practice to double book the time slot of someone with a high no show probability.
3. In direct primary care, many docs prefer to manually schedule because telemedicine or teletriage comes with the practice model. Most my patients will message me and I can take care of it over the phone. If I think they need to come in or if they want to come in I send them my availability and they pick a time like I would schedule a meeting or hang out with friends (or in some larger offices a front desk person does the scheduling). A lot of the complexity comes with the FFS model where a practice needs to see x number of people in order to generate enough revenue for each day. On that note, I would say the value based models may see much less complexity if done properly.
This is a great article that would benefit from a more empathetic take on why physicians change their schedule- the continual references to ditching patient care for a round of golf is a cheap laugh at at the expense of understanding what we ask physicians and APPs to manage during a typical patient care day. Yes, there are many obstacles but when you dig in and decide to make something better it is possible. I worked with a team that solved for direct patient scheduling which doubled self-scheduling within a year and nearly eliminated complaints of the wrong appointment being scheduled.